Regional psychiatric re-hospitalisation rates and their association with outpatient services
Background Psychiatric re-hospitalisation is dependent on patient level factors as well as health system level factors. Low re-hospitalisation rates are often considered a positive quality indicator in terms of mental health services. This study sets out to investigate psychiatric re-hospitalisation and its predictors on hospital district level in Finland.
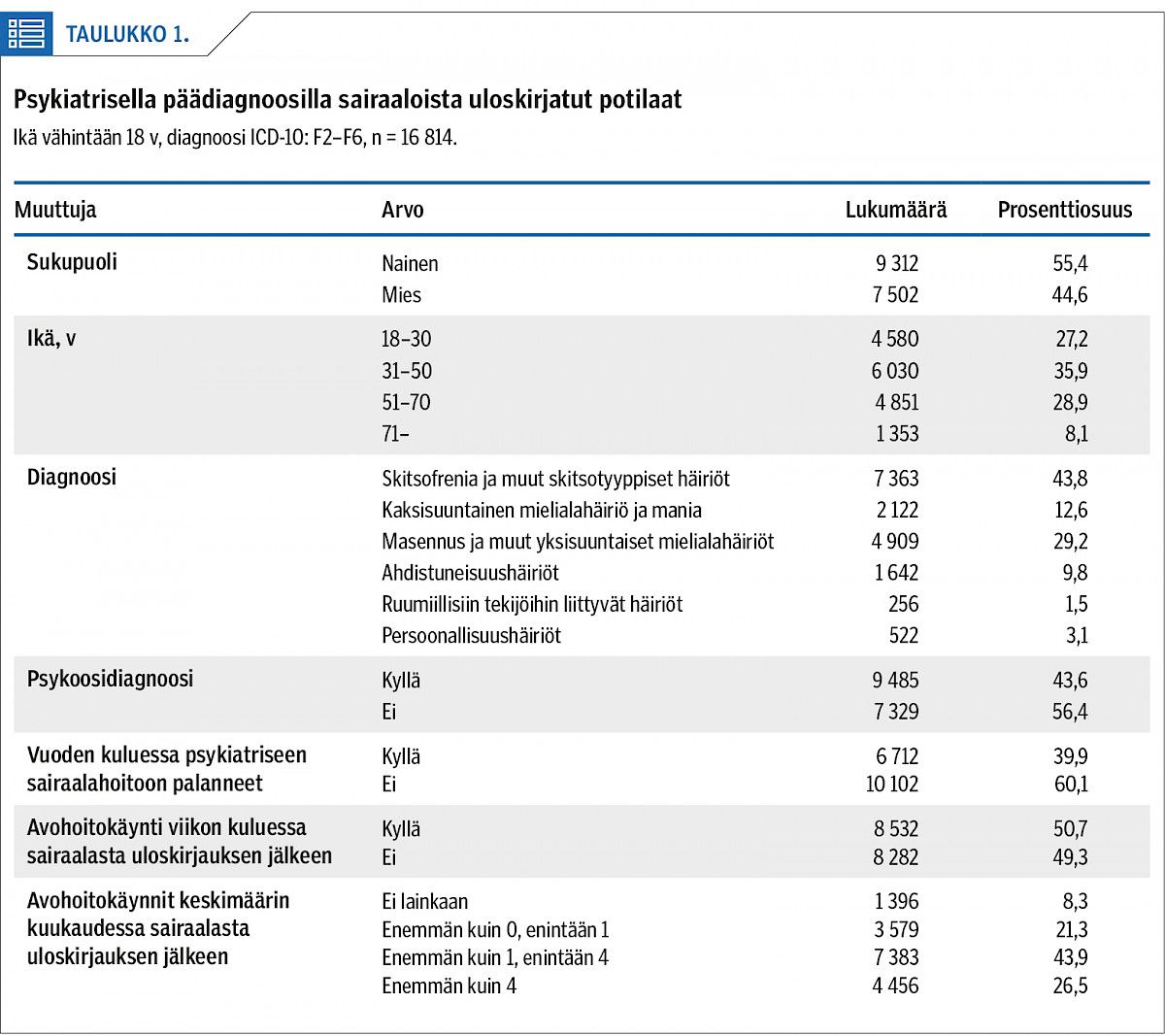
Methods The register-based study consisted of nationwide data on 16,814 adult patients (18–97 years of age) hospitalised with a psychiatric diagnosis (ICD-10 categories F2–F6) for a minimum period of 24 hours in the year 2012. Health service use was followed for 12 months, starting from date of discharge. Data were obtained from the Care Register for Health Care (Hilmo) and the Register of Primary Health Care Visits (AvoHilmo). Specialised and primary care outpatient contacts were examined. Statistical analysis was performed as frequency analysis and logistic regression with re-hospitalisation as the dependent variable.
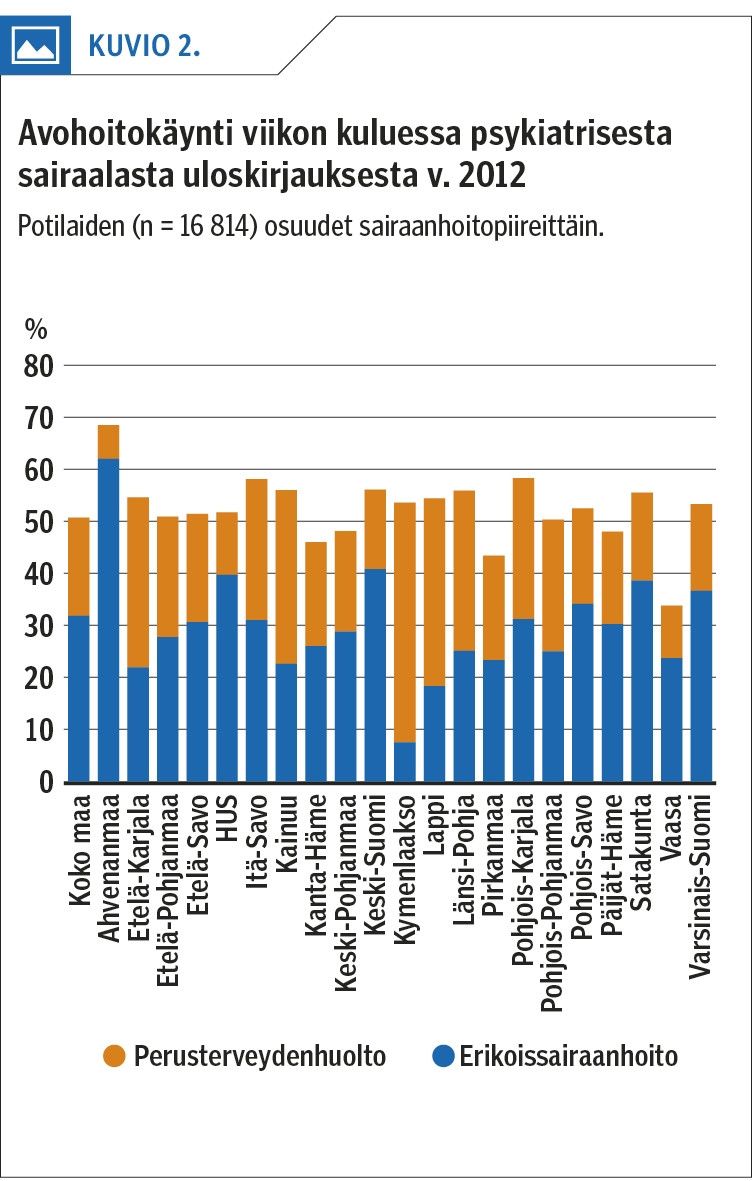
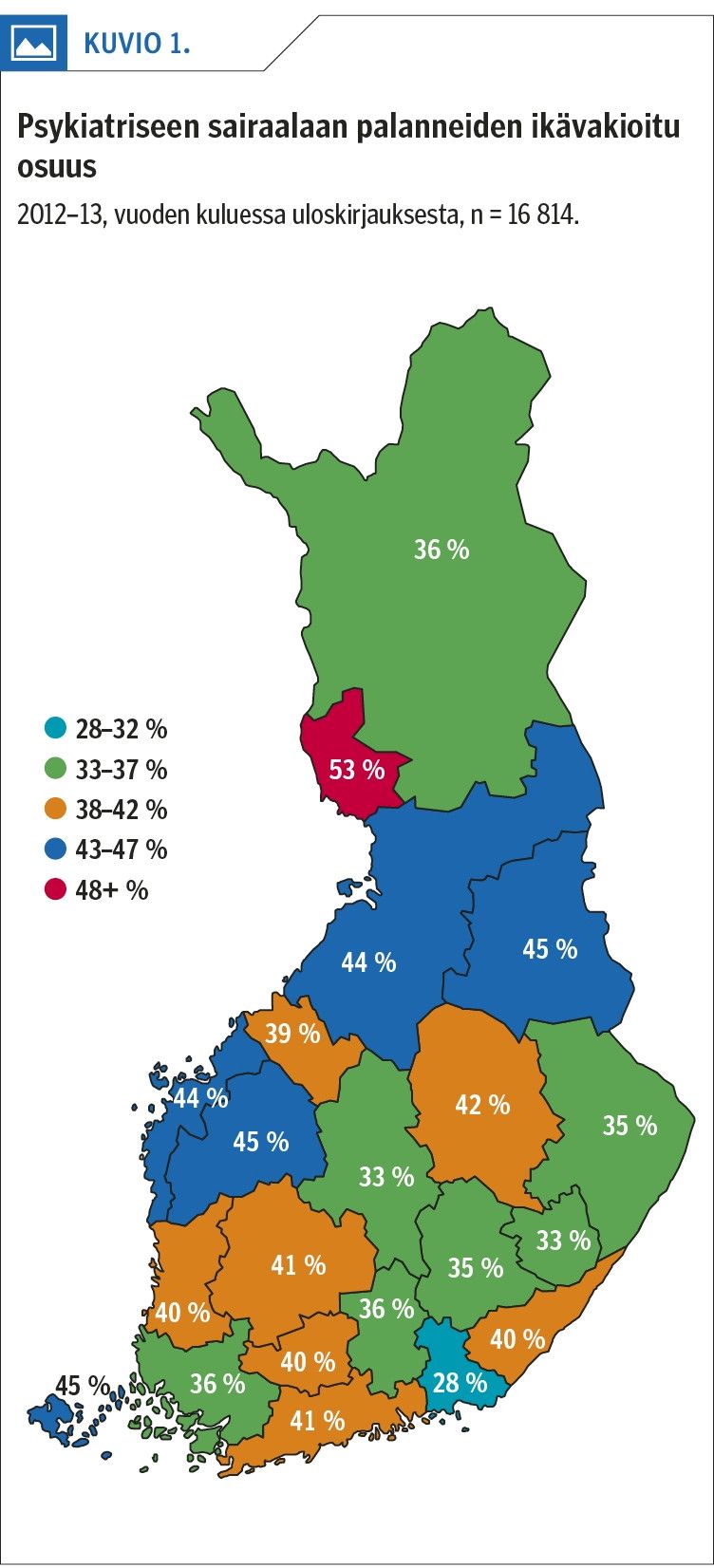
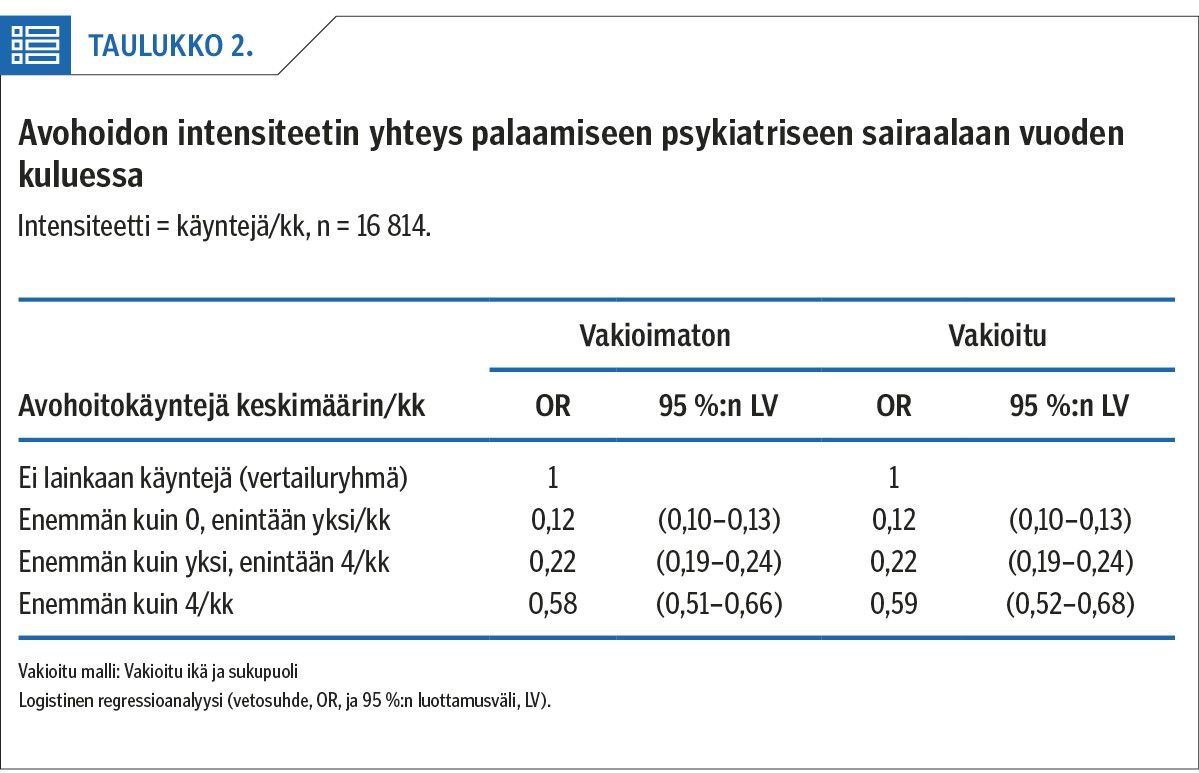
Results A total of 40% of patients were re-hospitalised into psychiatric inpatient care within a year (re-hospitalisation rate varying between hospital districts from 28–53%). Altogether 51% of patients received an outpatient appointment within one week from hospital discharge, while 8% received no outpatient contact at all during the 12-month follow-up. Typically, those who received outpatient care had 2.3 visits per month. The rate of psychiatric re-hospitalisation was highest for those who received no outpatient contact at all.
Conclusions Regional differences in psychiatric re-hospitalisation rates can to some extent be explained by health service organisation. Health services should direct more attention to the early weeks following hospital discharge. Even one contact with outpatient services resulted in a decreased risk of re-hospitalisation. Low levels of unplanned psychiatric re-hospitalisation rates, together with a seamless transition to outpatient services following discharge are both promising health service quality indicators. These indicators could benefit from regular regional follow-up.