Outcomes of transcatheter aortic valve implantation in Finland and benchmarking between Finland and Sweden
Background
Data demonstrating the outcome of transcatheter aortic valve implantation (TAVI) in Finland are lacking.
Methods
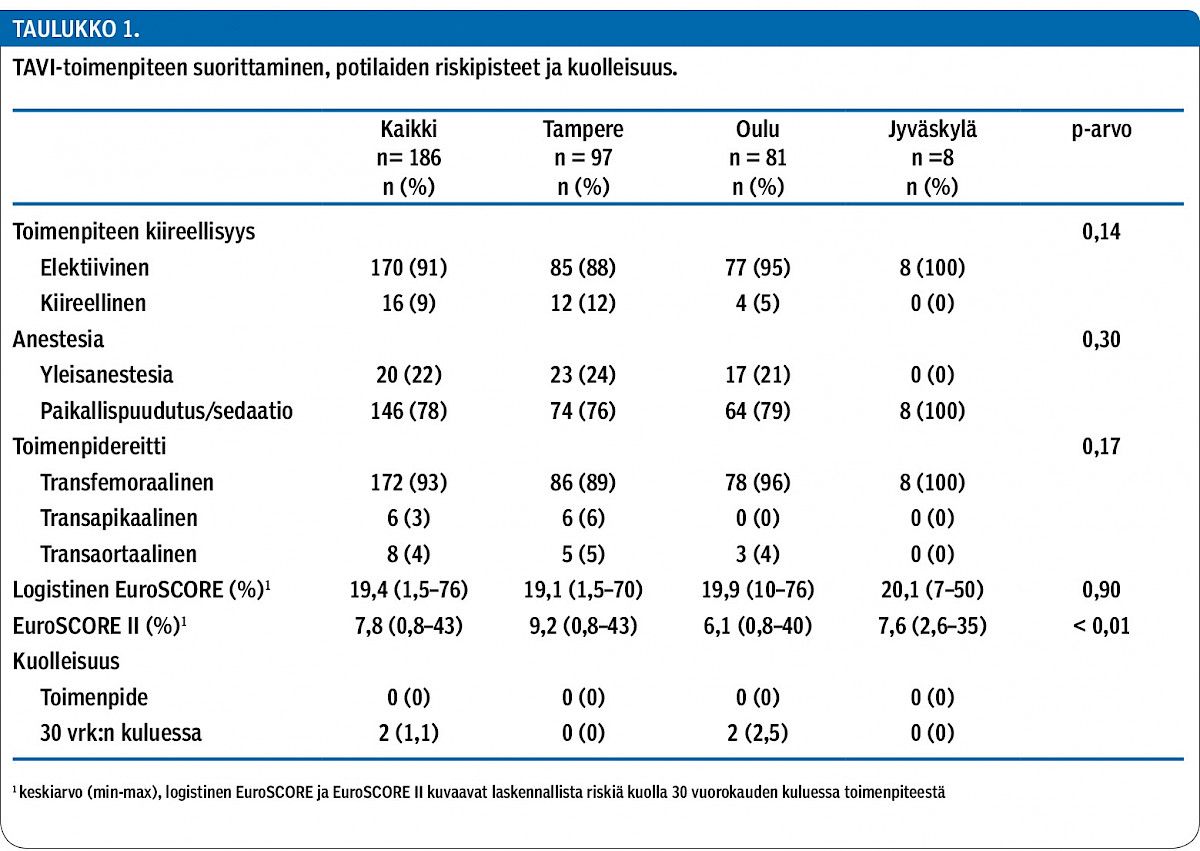
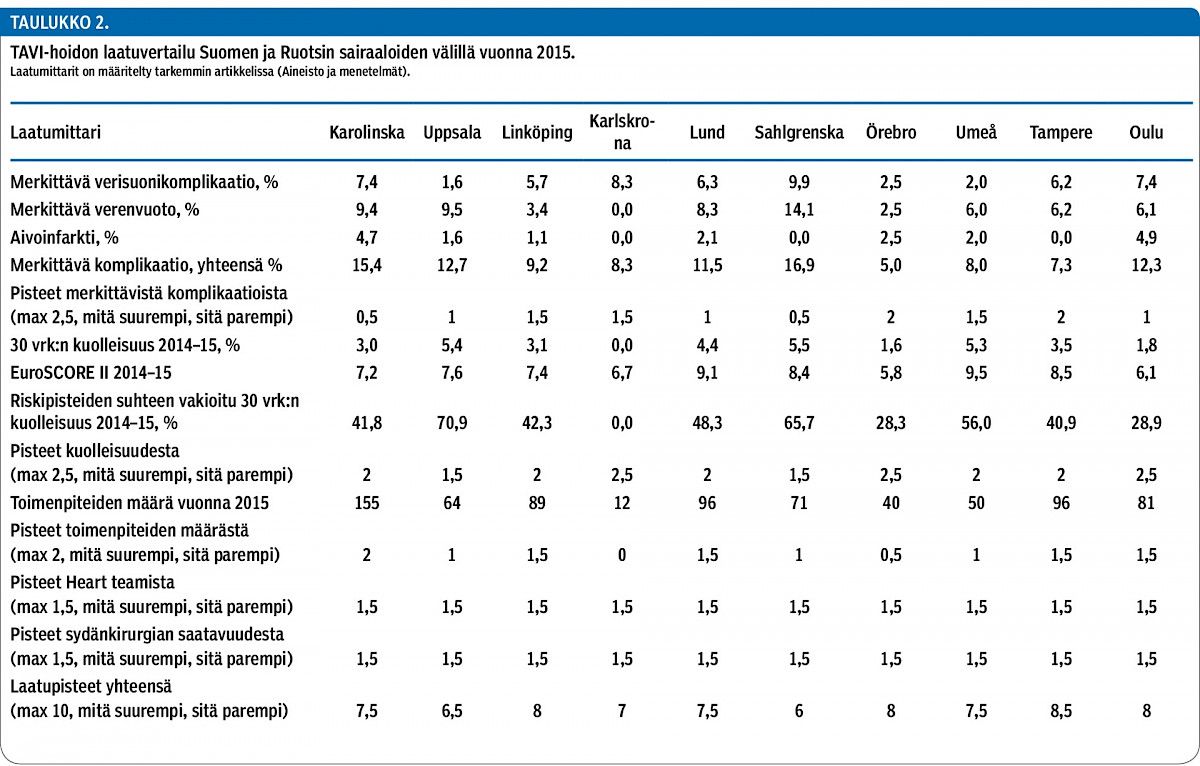
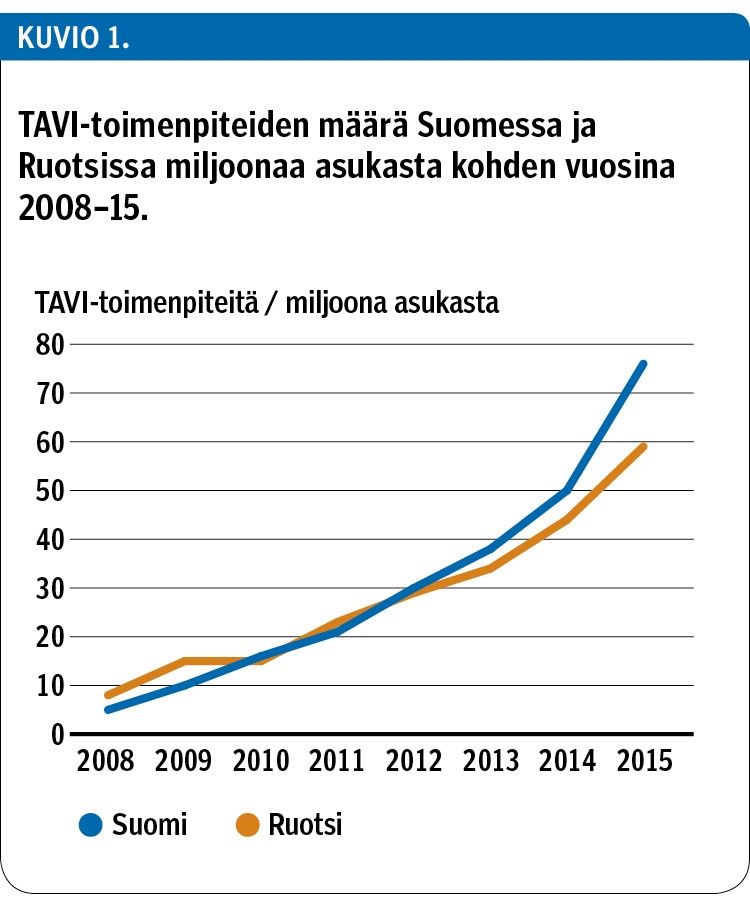
The KARDIO registry is a prospectively collected database in the 3 out of 6 centres performing TAVI procedures in Finland, and the Swedish Percutaneous Valve Registry includes all TAVI procedures from all eight TAVI-implanting centres in Sweden. These registries included 763 patients who underwent TAVI in 2015. All recorded variables were defined in accordance with the updated Valve Academic Research Consortium-2 (VARC-2) criteria. The outcomes of the hospitals were compared and the TAVI Quality Index per centre was calculated. In the benchmarking between Finland and Sweden the two preceding years’ (2014 and 2015) mortality rates were used to minimize fluctuations due to low case numbers.
Results
In Finland (n = 186) the median age was 83 years, 51% were females and the mean logistic EuroSCORE was 19.4%. The pre-operative aortic valve area was 0.6 ± 0.2 cm² with a median transvalvular gradient of 46 ± 15 mmHg. TAVI was performed percutaneously in the majority of patients (93%) while 14 (7%) procedures were done surgically: 6 (3%) using a transapical approach and 8 (4%) a transaortic approach. The majority of the procedures were performed under local anaesthesia or conscious sedation (78%). The 30-day death rate was 1.1% in Finland in 2015. The benchmarking analyses between hospitals in Finland and Sweden showed wide variation for major vascular complications (from 1.6 to 9.9%), major bleeding (from 0 to 14.1%) and stroke (from 0 to 4.9%). The 30-day mortality rate after TAVI in 2014–2015 ranged between 0 and 5.5%.
Conclusions
In this real-world TAVI registry of high-risk patients with aortic stenosis 30-day mortality was low. The major complication rate was acceptable considering the advanced age and frequent co-morbidities of the treated patients. However, there is wide variation in event rates between sites. By measuring and comparing baseline, procedural and outcomes variables it is possible to identify areas for improvement that will reduce variation and improve patient outcomes. These findings prove the importance of non-selective registries and support the utilization of TAVI in Finland and Sweden.