Hip problems in children and adolescents with cerebral palsy. Systematic radiographic follow-up is needed in Finland.

Background
Cerebral palsy (CP) is a group of disorders affecting an individual’s movement and posture, causing activity limitations that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain.
The yearly prevalence rate of CP is approximately 2‰. The disorder often requires regular rehabilitation by a multi-professional team, frequently continuing throughout the individual’s life. The heterogeneity of the brain damage influences the degree of motor impairment, co-morbidity, functional ability and prognosis.
The main goal of the study was to compare the follow-up of hip x-ray examinations in Finland to the standards set by the Nordic CPUP (Uppföljningsprogram för cerebral pares) programme.
Methods
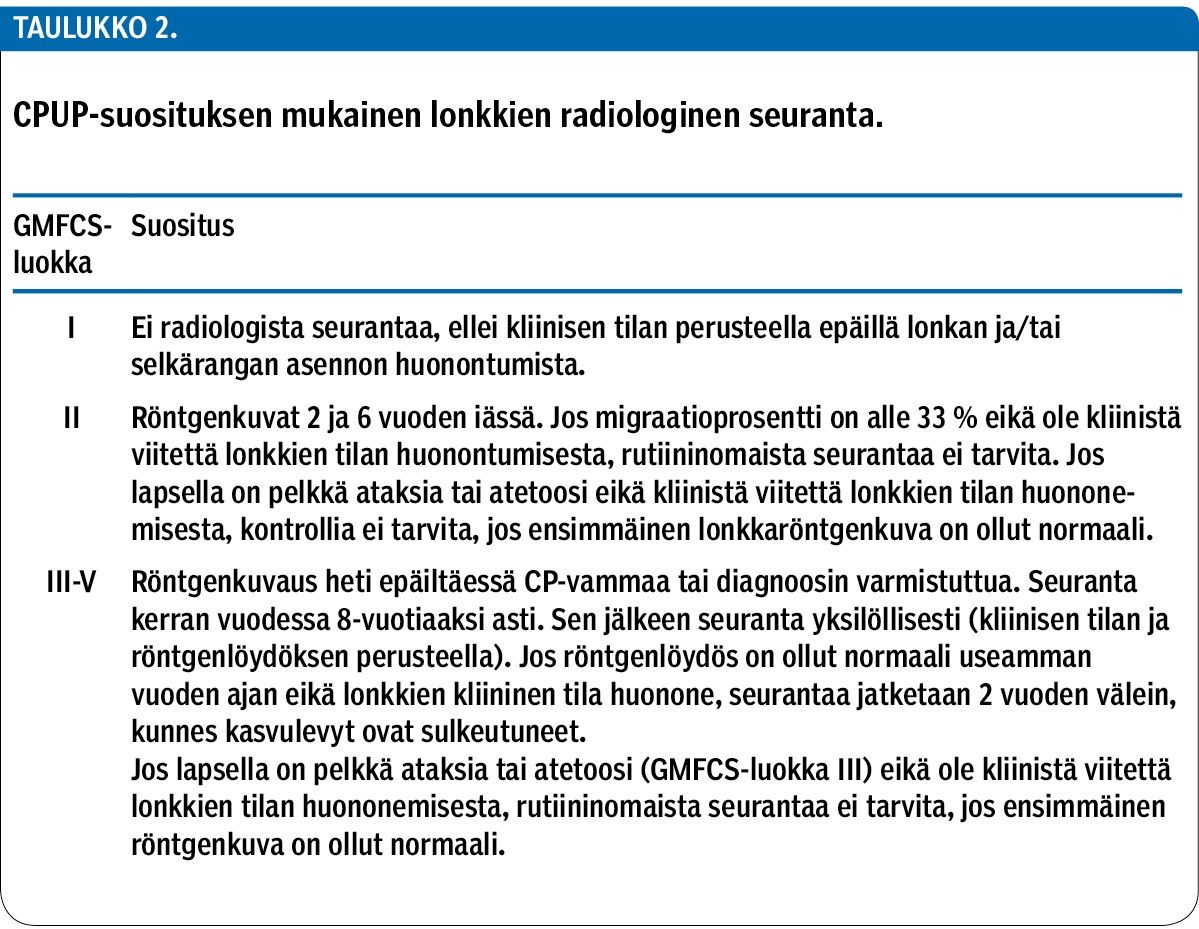
To investigate how the radiological follow-up of the hip x-ray examinations has been performed in Finland, we collected and analyzed medical records (first hip x-ray, medical report, surgical operations) of 362 children and adolescents participating in the national CP research programme. To further examine hip x-ray follow-up practices, we conducted a questionnaire survey among chief physicians of paediatric neurology.
Results
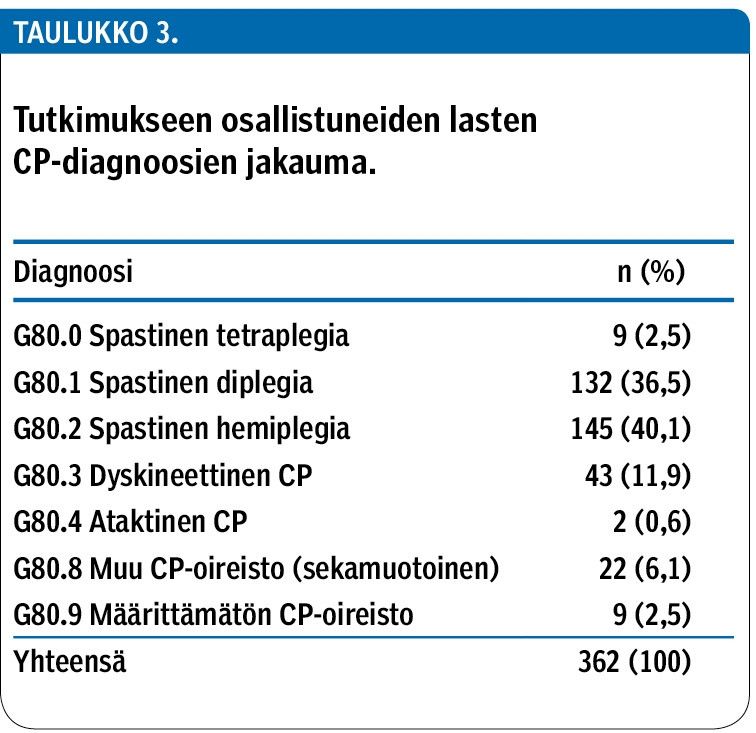
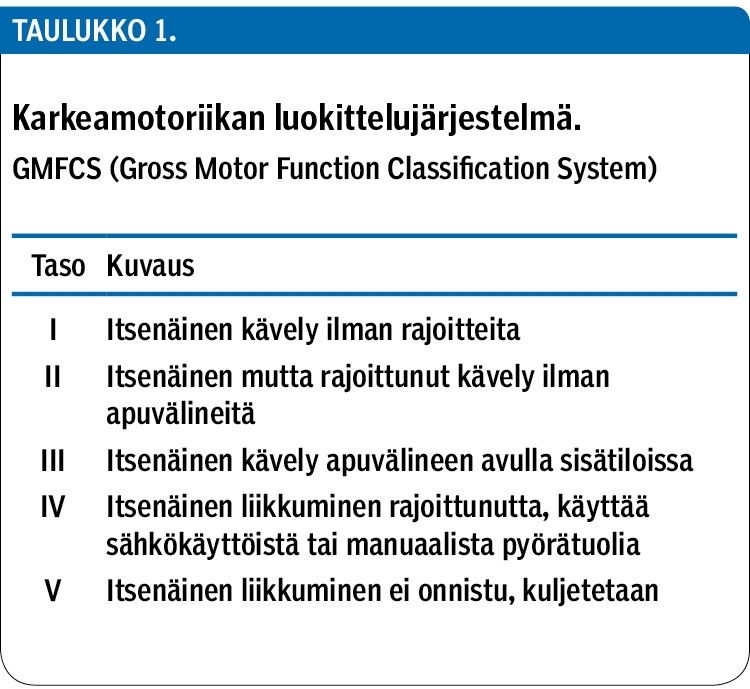
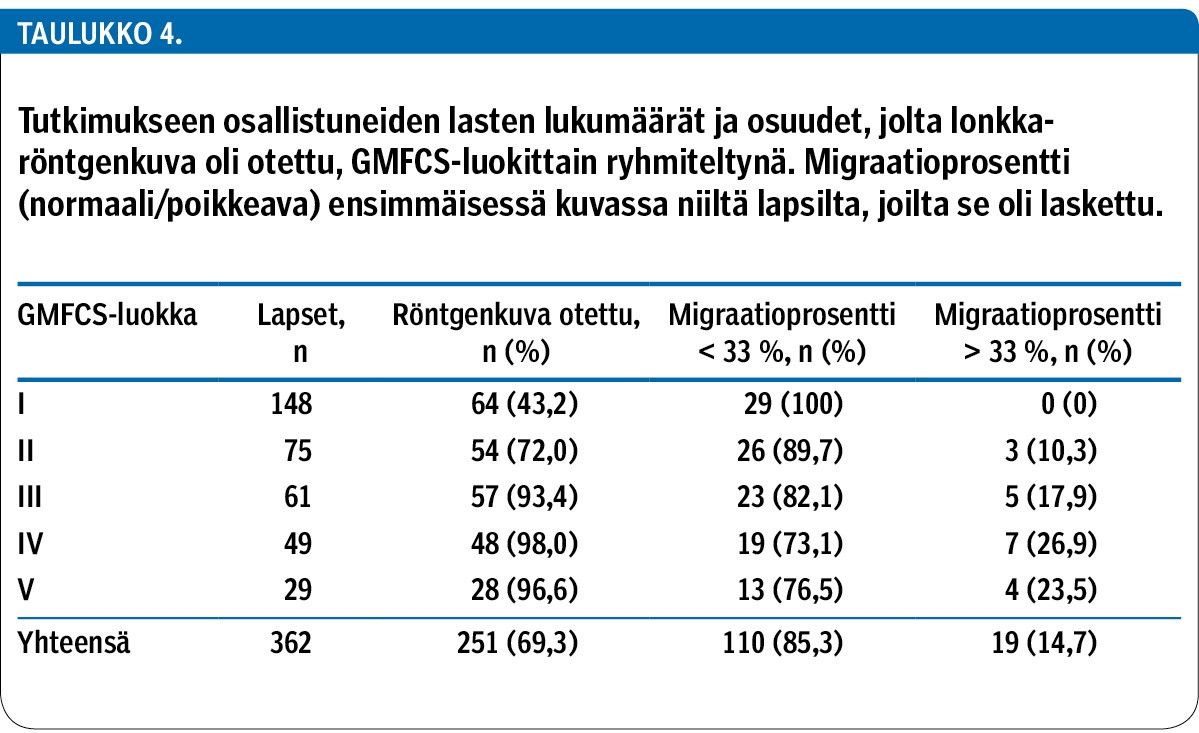
A total of 69% (N = 251) of the children had undergone hip x-ray examination at least once. The time of the first x-ray varied from 0.2 years to 15.2 years and the number of x-rays per child ranged from one to 22. According to the CPUP standards, no routine x-ray examinations are recommended for children with only minor limitations in mobility (Gross Motor Function Classification System, GMFCS Level I). In this study almost half (43%) of the children at this level of gross motor function had been examined at least once.
For children with limitation in mobility but no need for mobility aids (GMFCS II) x-rays are recommended at the ages of two and six years. For children utilizing mobility aids (GMFCS Levels III−V) the first hip x-ray is recommended to be taken as soon as the diagnosis is made. In this study one third (33%) of the children in this category were not examined until the age of three or above. Six children at this level of gross motor function had never had an x-ray examination.
Conclusions
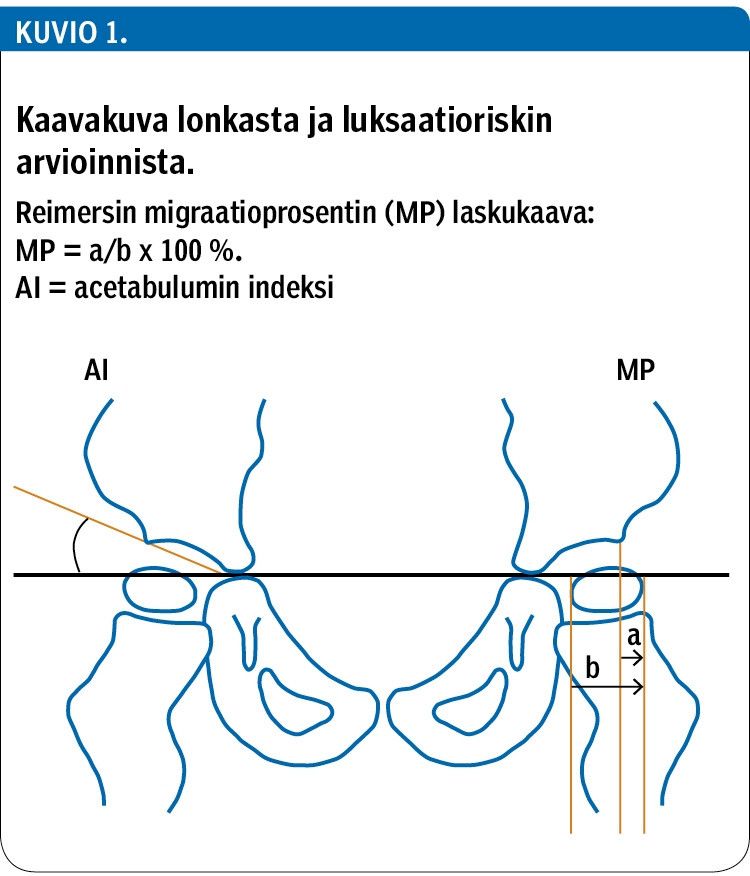
Hip x-ray follow-up practices for CP children and adolescents in Finland vary considerably by region and differ from the recommended CPUP follow-up surveillance programme. The radiologists’ reports commonly lacked measures for subluxation (such as the migration percentage). Striving towards more uniform practices in hip x-ray follow-up is important: performing radiological examinations at the right time allows for early intervention and aids in avoiding unnecessary radiological examinations.