English summary: Physical comorbidity and functional limitations in psychotic disorders in Finland

Background
Schizophrenia and other psychotic disorders are associated with increased risk of developing medical comorbidity and 2- to 3-fold risk of premature death from medical illnesses. A nationally representative sample allows a comparison of somatic disorders and functional capacity between persons with psychotic disorder and those without.
Methods
The Health 2000 study was based on a nationally representative survey of 8028 persons aged 30 or older. The fieldwork consisted of a home interview and a health examination. The Psychoses in Finland study is a substudy of the Health 2000 survey. Persons with possible psychotic disorder were screened and interviewed using SCID-I.
Results
The prevalence estimate of type 2 diabetes was significantly higher among subjects with schizophrenia or other non-affective psychotic disorders (ONAP) than in the general population. Users of all types of antipsychotic medication had increased prevalence of type 2 diabetes.
The criteria of metabolic syndrome were fulfilled more often in subjects with schizophrenia or ONAP than in those without psychotic disorder, though not statistically significantly. However, subjects with schizophrenia had significantly lower HDL cholesterol and higher triglyceride and glucose levels and larger waist circumference, but lower systolic blood pressure than the remaining study population.
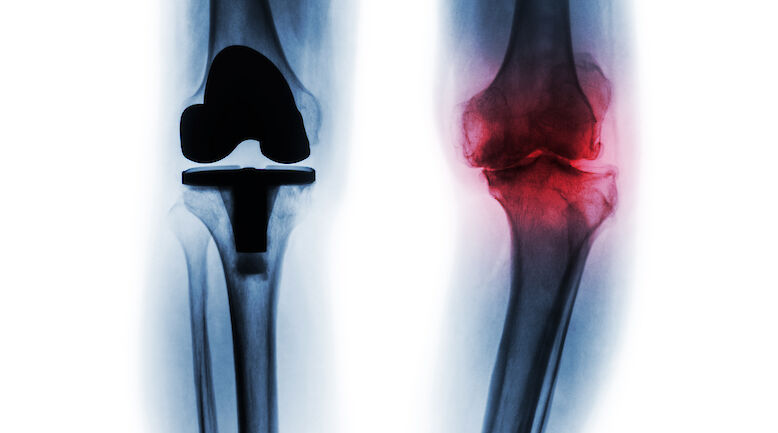
Coronary heart disease was not more common among subjects with psychotic disorder than in the general population, but large Q-waves suggesting past myocardial infarction were more frequent in subjects with schizophrenia. Schizophrenia was associated with obesity, abdominal obesity and high body fat percentage.
Women with schizophrenia and men with affective psychosis had significantly lower bone ultrasound values than the general population. Subjects with schizophrenia had also lower vitamin D levels, which is a risk for osteoporosis.
Both near and distant vision were reduced in subjects with schizophrenia but not in subjects with psychotic disorders. Self-reported problems with vision were more common in subjects with schizophrenia and vision had been examined less often during the previous 5 years than in subjects with other psychotic disorders.
Self-reported and test-based mobility limitations were highly prevalent in subjects with schizophrenia and ONAP as was weak muscle strength. Even participants under 55 years reported more difficulties in walking, stair climbing and running than the general population.
Schizophrenia and ONAP were associated with limitations in activities and instrumental activities of daily living as well as in social functioning. One significant predictor of problems was reduced vision, which at least in some situations could be easily corrected.
Subjects with schizophrenia had generalised cognitive impairment, while those with ONAP were impaired in verbal memory and processing. Schizoaffective disorder was associated with the largest loss of quality of life, with bipolar I disorder associated with similar or smaller loss than schizophrenia. Current depressive symptoms explained most of the loss of quality of life.
Conclusions
Medical problems and functional limitations were significantly more common in subjects with psychotic disorder than in the general population. Annual health examinations are necessary in order to more effectively discover these problems. More attention should be paid to active treatment of depression.